Estimated reading time: 6 minutes
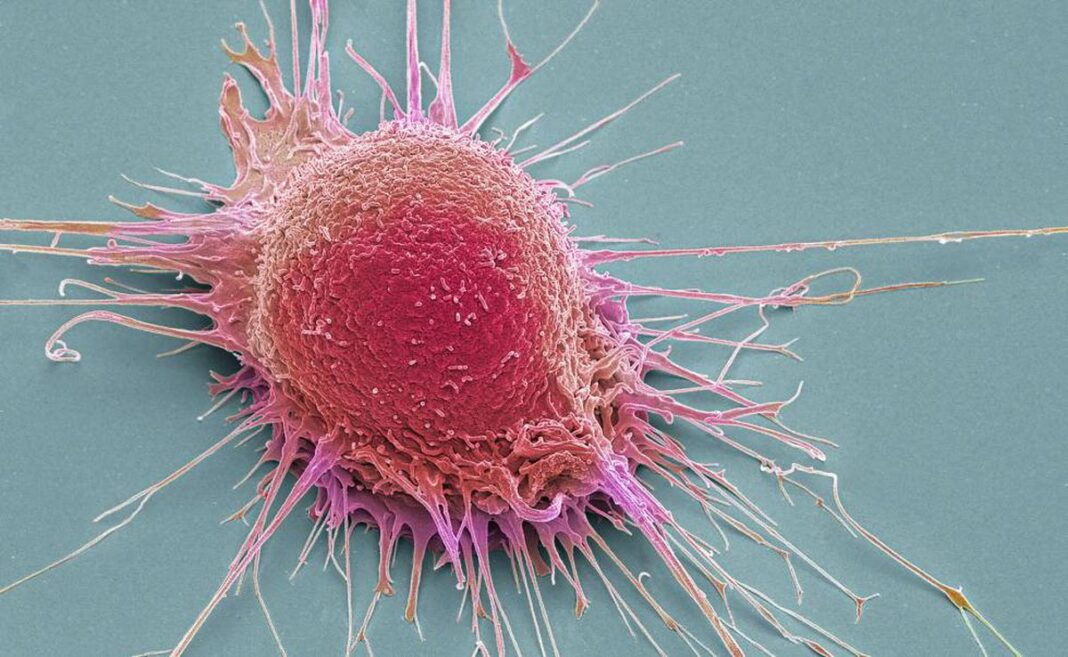
A new SALURBAL study published in The Lancet Global Health explores the complex relationship between cancer mortality rates and socioeconomic development in 343 cities across nine Latin American countries. The study, led by researchers at the Salud Urbana en América Latina – Urban Health in Latin America (SALURBAL) project, analyzed data from 2015 through 2019 to map the geographic distribution of cancer deaths for seven common types of cancer: breast, lung, colorectal, stomach, liver, prostate, and cervical. The findings provide valuable insights into the impact of socioeconomic factors on cancer outcomes in urban Latin America.
- According to the study, lung cancer accounted for 13 deaths for every 100,000 inhabitants across the cities included in this study. It was the leading cause of cancer mortality for both males and females in 214 out of 343 cities, resulting in a total of 186,480 deaths from 2015 to 2019.
- Cities with lower socioeconomic status exhibited higher mortality rates for cervical, liver, prostate, and stomach cancers. Conversely, in cities with higher socioeconomic levels, there were higher cancer mortality rates for breast, colorectal, and lung cancer.
- The associations between cancer mortality and lower socioeconomic development (most notable for cervical, stomach, and liver cancers) were stronger in women as compared with men, while cancers linked to higher socioeconomic status (for example, lung and colorectal cancers) had stronger associations in men.
- Rates of cancer-related mortality varied dramatically across cities: among men, from just over 63 per 100,000 inhabitants in San Miguel, El Salvador, to over three times higher (211 per 100,000) in Antofagasta, Chile. Among women, cancer-related mortality ranged from 62 per 100,000 inhabitants in Tecomán, Mexico to over twice as high (137 per 100,000) in Rio Grande, Brazil.
Cancer is the second leading cause of death worldwide. In 2022, Latin America reported 750,000 deaths due to this illness. The region faces high levels of both lifestyle-related and infection-related cancers, which are influenced by differing levels of socioeconomic development. Although policies and programs could be implemented to prevent and detect early cancer, socioeconomic inequality can pose challenges to these efforts.
Researchers from the SALURBAL project set out to analyze the relationship between city-level socioeconomic development and overall cancer mortality rates, as well as rates for seven specific types of cancer. The team used the Social Environmental Index (SEI) to approximate socioeconomic levels based on indicators such as educational attainment, overcrowding, and access to water and sanitation.
The five most common cancers in Latin America for both men and women were lung; stomach; colorectal; breast; and prostate.
Geographical distribution of overall age-standardized cancer mortality rates, by sex and city
Among females, breast cancer was the leading cause of cancer deaths across all socioeconomic levels. In poorer cities, cervical cancer ranked second, while lung and colorectal cancers were the second and third most common causes of cancer-related deaths in all other cities. For males, the patterns were more consistent across socioeconomic levels. Prostate cancer was the leading cause of cancer-related deaths in cities with low and medium-low socioeconomic levels and remained the most common cause in wealthier cities.
“Our results emphasize the importance of considering the local context when planning policies to fight against cancer”, says Tania Alfaro M.D., Assistant Professor of the Epidemiology Program at the Universidad de Chile and lead author of the study. “Particularly important is that most previous studies have focused on cities in North America and Europe or just a few cities in Latin America.
Now, we could study 343 cities from Latin America that present particular geographical patterns and different contextual risk factors, so these findings could be important to policy planners in Latin America.
The study found that cities with higher SEI had higher rates of lung, colorectal, and breast cancer compared to cities with lower SEI. Conversely, cities with lower SEI had higher proportions of liver and cervical cancer. Additionally, the impact of socioeconomic levels on cancer mortality varied by sex. For females, and compared to the poorest cities, those with the highest level of development (highest SEI) had 13% higher lung cancer mortality rates, compared to 22% in the case of men. Cancer-related mortality rates varied widely between different regions. For example, liver cancer mortality was generally low across the region except for Southern Mexico and Central America, where it was amongst the most common causes of cancer death.
The authors also found significant variation in some cancer-related mortality rates between cities in the same country. For females, cervical cancer rates showed a variability of 79% between cities in the same country, while within-country variability for other types of cancer ranged from 34% to 45%. In males, prostate cancer rates varied by 66% across cities in the same country.
“When we talk about global cancer, we usually focus on national numbers and differences between countries.” Says, Kevin Martínez, M.D., Postdoctoral Research Fellow at the Center for Global Health Equity of the University of Michigan and co-author of the study. “However, this paper highlights the variability in cancer rates within countries, showing that differences among subpopulations can be greater than national averages. It also reveals that social factors impact groups differently.”
For instance, among males, the highest mortality rates for lung, colorectal, and stomach cancer were concentrated in South America. The highest liver cancer mortality rates were primarily observed in cities in Mexico and Central America. Additionally, high mortality rates for stomach cancer, particularly among males, were found in Andean cities—specifically in Colombia and Chile.
“We see these differences, and we know they have an impact, even if this study doesn’t explain the causes of these discrepancies.” Says Dr. Alfaro, “These variations may reflect different stages of the epidemiological transition across cities, impacting men and women differently. For instance, the tobacco epidemic started first among men, before women. In my view, these differences could also be the result of a disparity in access to diagnosis and treatment, particularly for women in lower socioeconomic areas.”
Dr. Alfaro emphasizes the importance of continuing this type of research, which could inform action plans targeting inequities in specific cancers. Effective city policies and thoughtful urban design are crucial for promoting healthy lifestyles and reducing exposure to harmful factors like air pollution. By creating environments that include ample green spaces and facilitate healthcare access, cities can boost the effectiveness of preventive care and specialized cancer treatments, making a real difference in community health. However, addressing socioeconomic inequalities is key to ensuring these benefits reach all community members.
The study underscores the need for targeted efforts to manage cancer risk factors, improve early diagnosis and treatment, and address inequities across Latin America. Findings like these can inform strategies to reduce the cancer burden, especially among vulnerable groups.
Read the full study:https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(24)00446-7/fulltext
(https://drexel.edu/lac/media/news/2025/February/cancer-mortality-socioeconomic/)